Understanding Hysterectomy Surgery Risks: A Complete Guide by Leading Obstetricians & Gynecologists at Dr. Seckin
When it comes to women's health, surgical procedures such as hysterectomy are often critical for addressing a variety of gynecological conditions. Although hysterectomy can significantly improve quality of life, it also involves inherent risks that every woman should understand thoroughly. This comprehensive guide aims to shed light on hysterectomy surgery risks, providing valuable insights into the procedure, potential complications, safety measures, and expert recommendations from top obstetricians and gynecologists at Dr. Seckin.
What is a Hysterectomy and Why Is It Performed?
A hysterectomy is a surgical operation that removes a woman's uterus, sometimes including surrounding structures such as the cervix, ovaries, and fallopian tubes. It is one of the most common gynecological surgeries worldwide, performed to treat various conditions including uterine fibroids, endometriosis, abnormal bleeding, uterine prolapse, cancer, and chronic pelvic pain.
Hysterectomy options vary depending on the patient’s condition:
- Partial (subtotal or supracervical) hysterectomy: removal of the uterus while leaving the cervix intact.
- Complete hysterectomy: removal of the entire uterus and cervix.
- Radical hysterectomy: removal of the uterus, tissue around the uterus, part of the vagina, and possibly lymph nodes, usually performed in cancer cases.
Understanding the different types is essential when considering hysterectomy surgery risks, as each procedure has distinct risk profiles and recovery implications.
Common Reasons Leading to Hysterectomy Surgery
Before delving into the risks, it's important to recognize why hysterectomy might be the best or necessary option:
- Uterine fibroids: benign tumors causing pain, heavy bleeding, and pressure symptoms.
- Endometriosis: tissue similar to uterine lining growing outside the uterus, causing pain and infertility.
- Uterine prolapse: descent of the uterus into the vaginal canal due to weakened pelvic floor muscles.
- Abnormal uterine bleeding: heavy or irregular bleeding unresponsive to medication.
- Gynecologic cancers: including uterine, cervical, or ovarian cancer.
- Chronic pelvic pain: persistent pain not manageable with other treatments.
Understanding the Hysterectomy Surgery Risks
Despite its frequency and relative safety, hysterectomy is major surgery, and like all surgical procedures, it involves potential risks and complications. Recognizing these risks enables patients to make informed decisions and collaborate effectively with their healthcare providers. Below, we provide a detailed analysis of the hysterectomy surgery risks.
1. Anesthesia Risks
Generally performed under general anesthesia, hysterectomy carries inherent anesthesia risks, including allergic reactions, respiratory issues, or cardiovascular problems. An anesthesiologist thoroughly evaluates each patient to minimize these risks.
2. Bleeding and Hemorrhage
One of the primary hysterectomy surgery risks involves intraoperative or postoperative bleeding. Although surgeons take meticulous precautions, unforeseen bleeding can occur, sometimes necessitating additional interventions or transfusions.
3. Infection
Postoperative infections affecting the surgical site, pelvic cavity, or urinary tract are potential complications. Proper sterile techniques and postoperative care reduce this risk significantly.
4. Damage to Surrounding Organs
Because hysterectomy involves operating near critical structures, there exists a risk of accidental injury to adjacent organs such as the bladder, ureters, or intestines. Advanced surgical techniques and imaging guidance have significantly minimized these risks.
5. Blood Clots
Postoperative immobility can increase the risk of deep vein thrombosis (DVT) or pulmonary embolism (PE). Prophylactic measures, including early mobilization and blood thinners, are standard protocols to prevent such life-threatening complications.
6. Hormonal Changes and Menopause Symptoms
If ovaries are removed during hysterectomy, women experience an abrupt onset of menopause symptoms, including hot flashes, night sweats, mood swings, and decreased libido. Managing these symptoms requires appropriate hormonal therapy and lifestyle adjustments.
7. Psychological Impact
Hysterectomy can influence emotional well-being, causing feelings of loss or depression. Psychological counseling and support groups are invaluable resources for women navigating these emotional changes.
8. Future Pregnancy Implications
Post-hysterectomy, pregnancy is no longer possible. This significant consideration must be discussed beforehand, especially for women desiring future children.
Reducing and Managing Hysterectomy Surgery Risks
While risks are inherent, many complications can be mitigated through careful planning and skilled surgical techniques. Here are essential strategies:
- Comprehensive preoperative evaluation: including medical history, physical examination, and necessary imaging.
- Choosing an experienced surgeon: specialized in gynecological surgeries reduces intraoperative risks.
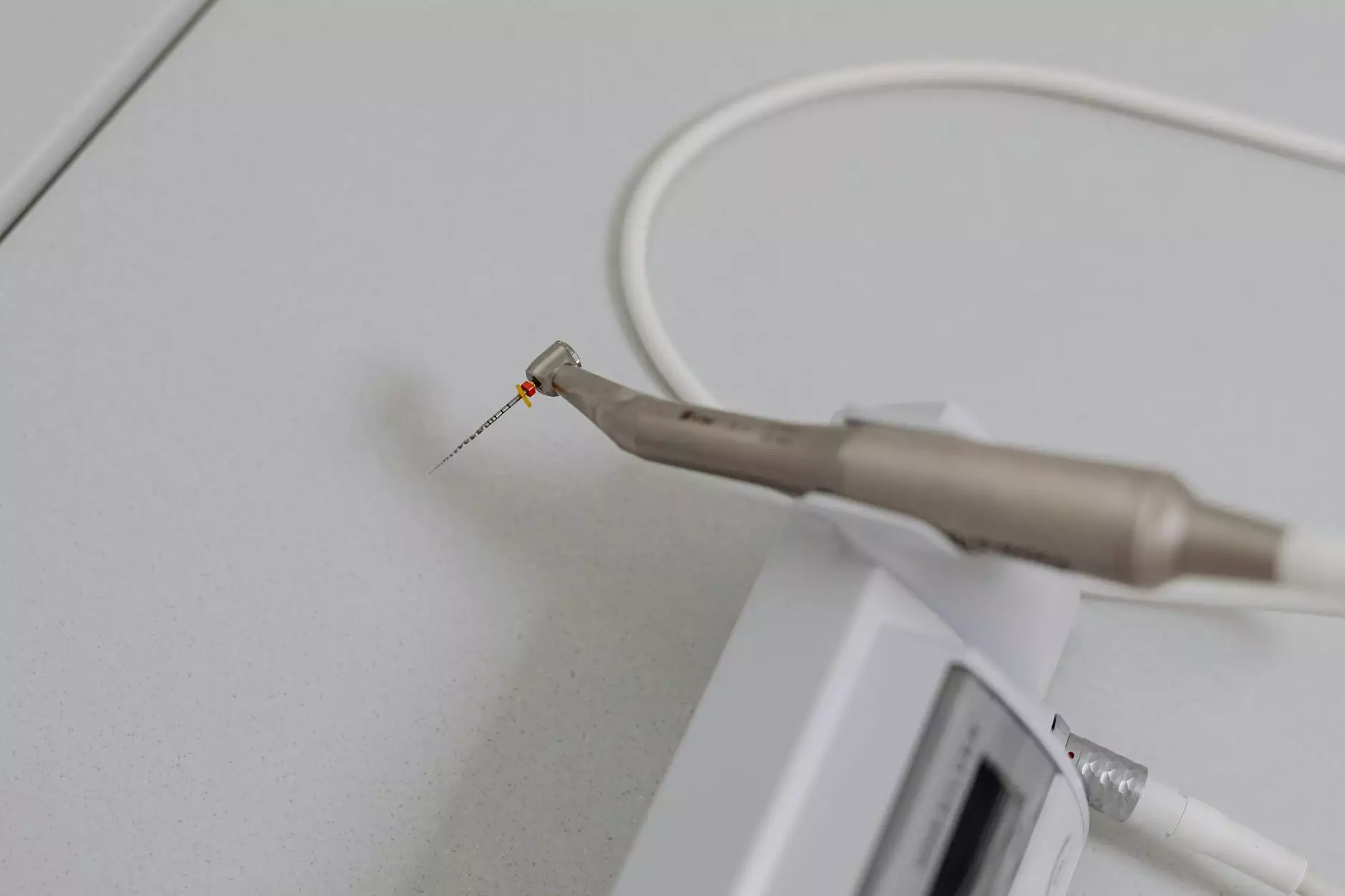
- Opting for minimally invasive techniques: such as laparoscopic or robotic-assisted hysterectomy, which tend to have fewer complications and quicker recovery.
- Adherence to sterile protocols: to minimize postoperative infections.
- Postoperative care and monitoring: including early mobilization, wound care, and timely recognition of complications.
The Critical Role of Patient Education and Consultation with Experts at Dr. Seckin
At Dr. Seckin, a team of highly proficient obstetricians & gynecologists emphasizes patient education. They ensure every woman comprehensively understands the hysterectomy surgery risks, alternative treatments, and postoperative expectations. This approach empowers women to participate actively in their healthcare decisions.
Choosing the Right Healthcare Provider for Safe Hysterectomy Procedures
Set yourself up for a successful surgery by selecting a provider renowned for excellence in women's health and surgical expertise. Leading clinics like Dr. Seckin’s practice combine state-of-the-art technology, personalized care, and extensive experience to optimize safety and outcomes.
Final Thoughts: Making Informed Decisions About Hysterectomy
While hysterectomy surgery risks are present, advances in surgical techniques, preoperative evaluations, and postoperative care have considerably enhanced safety profiles. The key to minimizing risks lies in comprehensive planning, choosing experienced surgeons, and maintaining open communication. Consulting carefully with trusted healthcare professionals ensures women receive tailored treatment that aligns with their health goals and personal circumstances.
Contact Dr. Seckin for Expert Gynecological Care
If you are considering a hysterectomy or need expert guidance on gynecological health, contact the specialists at Dr. Seckin. Our team is dedicated to providing compassionate, comprehensive care with a focus on safety, safety, and optimal outcomes.









